In Edward Yang’s film Yi Yi, an elderly woman falls into a coma following an accidental fall. Her caregiver advises the family to talk to her daily to aid recovery. But does speaking to a comatose individual truly make a difference? Can such patients actually hear, or even retain any degree of consciousness?
1. Conscious Responses in the “Vegetative State”
The question of whether comatose individuals retain consciousness has sparked debate since the 1990s.
Modern medicine traditionally defines the vegetative state as a condition characterized by a lack of conscious awareness and unresponsiveness. Yet, research indicates that 13–19% of patients diagnosed with VS or coma exhibit conscious responses to external stimuli.
▷ Owen, Adrian M., et al. “Detecting awareness in the vegetative state.” science 313.5792 (2006): 1402-1402.
A groundbreaking 2006 study published in Science (Owen et al., 2006) reported a compelling case [1]: a 23-year-old female patient in a vegetative state following a traffic accident demonstrated neural activity indistinguishable from that of healthy individuals when exposed to linguistic stimuli. Strikingly, when presented with sentences containing ambiguity, her left ventrolateral prefrontal cortex displayed neural responses typical of language comprehension.
Even more remarkably, the patient exhibited evidence of “imaginative behavior.” When instructed to imagine specific actions such as playing tennis or walking (motor imagery), her neural activity was indistinguishable from that of healthy controls.
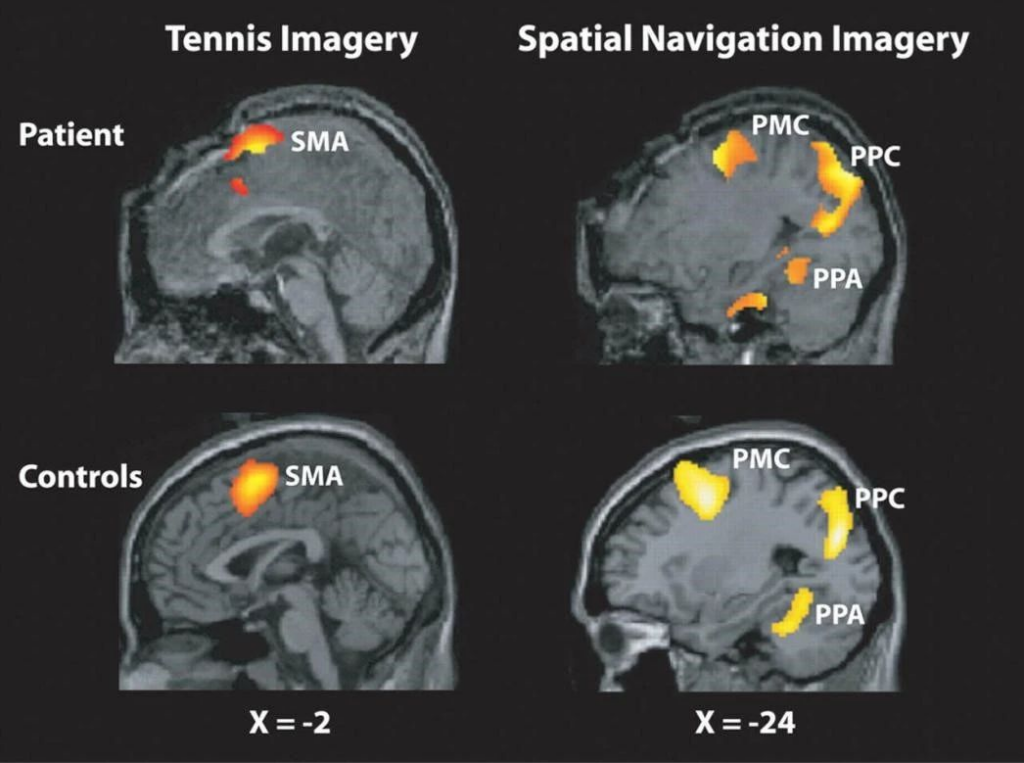
▷ The study monitored the activity of the supplementary motor area (SMA) in both the patient and a control group of 12 healthy volunteers during the process of imagining playing tennis. When imagining moving around her home, the researchers detected neural activity in the parahippocampal gyrus (PPA), posterior parietal cortex (PPC), and premotor cortex (PMC).
Despite meeting the clinical criteria for a vegetative state, her ability to comprehend and follow instructions suggested a preserved awareness of herself and her environment. This study underscored that neural activity in response to stimuli can serve as a marker of consciousness, while its absence does not necessarily confirm unconsciousness.
Previously, it was widely believed that comatose patients either progressed to brain death or transitioned into a vegetative state—both thought to lack consciousness entirely. However, Adrian Owen’s findings introduced the possibility of intermediary states, such as the “minimally conscious state” (MCS) or “covert consciousness.”
This raises a profound question: how can we accurately determine whether a person, especially one unable to communicate verbally or behaviorally, retains consciousness?
2. Determining the Presence of Consciousness
To assess the presence of consciousness in individuals with severe neurological conditions, it is crucial to first understand the classifications of death. Death is generally divided into two main categories: legal death (the cessation of legal personhood) and natural death, which itself encompasses three progressive stages: clinical death, brain death, and biological death [2].
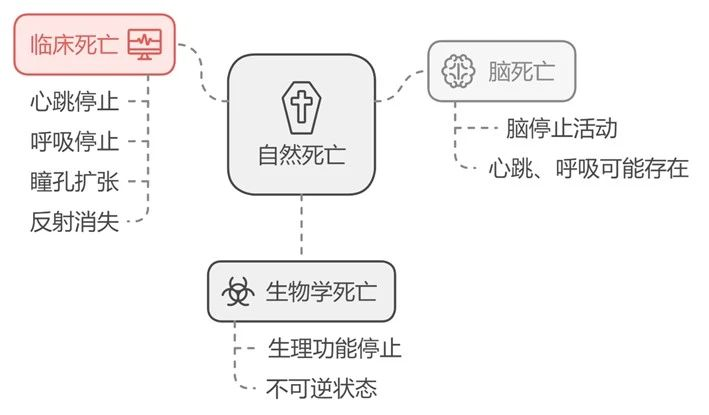
The vegetative state (VS) is a condition that resembles these stages but retains certain physiological functions. According to the Merck Manual of Diagnosis and Therapy [3]:
The vegetative state is a chronic condition in which patients can sustain blood pressure, respiration, and cardiac functions but lack higher cognitive abilities. While the hypothalamus and medullary brainstem functions remain intact to support cardiopulmonary and autonomic systems, the cortex suffers severe damage, eliminating cognitive function. Despite this, the reticular activating system (RAS) remains functional, allowing wakefulness. Midbrain or pontine reflexes may or may not be present. Typically, such patients lack self-awareness and interact with their environment only via reflexive responses.
However, findings from Owen’s team demonstrate that patients diagnosed as being in a vegetative state may indeed possess self-awareness and can even interact with their environment autonomously through neural activity. For example, patients have been shown to imagine actions, such as playing tennis, in response to instructions from clinicians. This neural activity, which can be detected using fMRI or EEG, indicates the presence of consciousness despite the absence of observable physical behavior. This phenomenon is referred to as “covert consciousness.”
3. Cognitive-Motor Dissociation: A New Understanding of Consciousness
Building on Adrian Owen’s groundbreaking research, subsequent studies have confirmed the phenomenon of “covert consciousness” in patients previously classified as being in a vegetative state. These findings, often based on motor imagery techniques, have identified a condition termed Cognitive-Motor Dissociation (CMD).
CMD describes a state in which patients demonstrate measurable neural responses to external stimuli, including motor imagery comparable to that of healthy individuals. However, due to motor system impairments, they are unable to execute corresponding physical actions.

▷ Schiff, Nicholas D. “Cognitive motor dissociation following severe brain injuries.” JAMA neurology 72.12 (2015): 1413-1415.
In 2015, Nicholas D. Schiff’s team used advanced imaging techniques such as Dynamic Causal Modeling (DCM) and Diffusion Tensor Imaging (DTI) to assess the functional integrity of brain networks supporting motor imagery in these patients. Their research aimed to uncover the neural mechanisms underlying Cognitive-Motor Dissociation [4].
The study revealed that in healthy individuals, excitatory coupling between the thalamus and motor cortex is critical for executing motor behaviors. However, in patients with covert consciousness, analyses using DCM and DTI demonstrated a selective disruption of this coupling. This disruption explains the dissociation between preserved motor imagery and absent skeletal movement. It is akin to operating the mechanical arm of an excavator when the circuit between the control panel and the arm is severed—you can still issue commands, but the arm cannot carry out the movements.
*DCM: A neuroimaging technique that examines causal relationships and connectivity between brain regions, providing insights into their functional interactions.
DTI: An MRI-based method for mapping the direction and integrity of white matter tracts, offering a detailed view of brain structural connectivity and its changes.
4. Research on the Prevalence of Cognitive-Motor Dissociation
Patients with Cognitive-Motor Dissociation (CMD) are often misdiagnosed as being in a vegetative state. However, there is currently no standardized method for accurately identifying CMD. The mechanism identified by Schiff’s team, discussed earlier, may not apply universally to all CMD cases. Moreover, previous studies on CMD have generally been small-scale, fragmented, and lacking consistency, with limited sample sizes. Under these conditions, developing a globally applicable standard for patient assessment is challenging, let alone designing targeted treatment approaches for CMD.
To address this issue, the paper titled “Cognitive Motor Dissociation in Disorders of Consciousness”, [5] supported by the Tianqiao Chen Institute-MGH Research Scholar Award, offers a potential solution. This study, published in The New England Journal of Medicine in August 2024, features Chen Scholar Brian L. Edlow as a key participant.
▷ Bodien, Yelena G., et al. “Cognitive motor dissociation in disorders of consciousness.” New England Journal of Medicine 391.7 (2024): 598-608.
This study recruited patients from diverse settings, including intensive care units, rehabilitation centers, nursing homes, and community populations. A unified inclusion criterion was applied: participants had no prior history of neurological or psychiatric disorders and were physiologically capable of undergoing brain imaging techniques, including MRI and EEG.
The research analyzed 353 adult patients diagnosed with disorders of consciousness using motor imagery tasks assessed via fMRI and EEG. Among these, 241 patients were classified as being in a coma, a vegetative state, or a minimally conscious state (MCS) based on the internationally recognized Coma Recovery Scale-Revised (CRS-R). Notably, 25% (60 patients) of this group exhibited CMD, characterized by task-based neural responses despite the absence of behavioral responses. Additionally, 112 patients were diagnosed as being in an MCS+ state or as having recovered from MCS. Among this subgroup, 43 patients (38%) exhibited observable task-based responses to commands detected via fMRI, EEG, or both.
*Minimally conscious states are further categorized as MCS− and MCS+, based on language processing abilities: MCS+ patients demonstrate simple command-following, intelligible verbal expression, or conscious but non-functional communication. MCS− patients exhibit more limited behaviors, such as visual pursuit, localization to noxious stimuli, or basic spontaneous activities like grasping bedsheets.
This study reported a higher prevalence of CMD (25%) than previous research, which estimated that 10–20% of patients with disorders of consciousness exhibit CMD symptoms. While traditional behavioral metrics like CRS-R offer valuable insights into assessing patient consciousness and responsiveness, task-based neuroimaging technologies significantly enhance diagnostic accuracy. Notably, the combined use of EEG and fMRI further improves measurement precision. These findings suggest that the prevalence of CMD may have been underestimated in prior studies.
5. The Significance of Measuring Consciousness in the Vegetative State
Imagine being aware of everything around you—the hum of medical equipment by your bedside, the whispers of family and friends—yet being unable to speak, move, or respond in any way. This state of isolation and helplessness could lead one to abandon even the faintest will to live. Although the phenomenon of “living dead” occurs in only a minority of vegetative state patients, every individual, no matter how rare their condition, represents a unique and precious life.
Whether driven by technological advancement or humanistic ethics, we need a measurement method that is more accessible, precise, and cost-effective to determine the consciousness state of comatose patients. The research conducted by Y.G. Bodien and colleagues stands out by integrating patient data from multiple locations and unifying measurement methodologies through brain imaging techniques. This unprecedented approach has maximized the accuracy of identifying Cognitive-Motor Dissociation (CMD) patients and pointed the way forward for future medical technologies and treatments. Most importantly, it offers a renewed sense of hope to those trapped in a silent world.
[1] Adrian M. Owen et al.,Detecting Awareness in the Vegetative State.Science313,1402-1402(2006).DOI:10.1126/science.1130197
[2] Liao Youmou,Wang Xinde. Death? Brain Death? Clinical Death?[J]. CHINA TERMINOLOGY.
[3] MSD Manuals. 2024.09. https://www.msdmanuals.cn/professional/neurologic-disorders/coma-and-impaired-consciousness/vegetative-state-and-minimally-conscious-state
[4] Schiff ND. Cognitive Motor Dissociation Following Severe Brain Injuries. JAMA Neurol. 2015 Dec;72(12):1413-5. doi: 10.1001/jamaneurol.2015.2899. PMID: 26502348.
[5] Bodien, Yelena G et al. “Cognitive Motor Dissociation in Disorders of Consciousness.” The New England journal of medicine vol. 391,7 (2024): 598-608. doi:10.1056/NEJMoa2400645